OSTEOPOROSIS
DEFINITION: A systemic skeletal disease characterized by low bone mass and micro-architectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture (Consensus Development Conference for Osteoporosis – 1991).
NEWER THOUGHT: Osteoporosis is a skeletal disorder characterized by compromised bone strength (means bone density & bone quality) predisposing to an increased risk of fracture (NIH Consensus Conference).
Osteoporosis is most of the time a SILENT DISEASE. Symptomatic (painful) Osteoporosis is usually secondary to a primary cause (Eg.: Osteomalacia). Any fracture cannot be “Osteoporotic fracture” because, for it to be so, it has to be a “fragility fracture” with low BMD Scores (Fragility fracture is one which occurs with a fall from standing height or less – i.e. with trivial trauma).
Bone is a live, metabolically active tissue having cells, proteins & minerals. A cycle of bone resorption (Osteoclast – Mediated) & bone formation (Osteoblast – Mediated) is always on. From birth to 3rd decade is a positive balance with more & more formed. Then from age of 30 to death is a downgrade cycle. Peak bone mass (maximum calcium & protein in the bones) is achieved at 25-30 years of age in each individual’s life (peak bone mass achieved in trochanter is mid-teens, femoral neck is late-teens and spine is early-20s). Up to 10% of the skeleton is being remodeled at any one time. Cancellous bone has less mass (20%) but larger surface area (80%) and higher turnover each year (25%), whereas cortical bone has 80% mass and lesser surface area (20%) & only 3% turnover per year.
Types of Osteoporosis:
- Post-Menopausal (Occurring in females after menopause due to estrogen protection being taken away from bones)
- Senile Osteoporosis (Occurring in both sexes after 65 years of age)
- GIOP (Glucocortoid induced Osteoporosis)
- Others (Secondary to other factors): Eg. Hormonal, Drug induced, Osteomalacia, Hyper-Parathyroidism, GI Tract disorders, Marrow based disorders, etc.
WHO Classification for Post-Menopausal Osteoporosis through T-Score (It is standard deviation of BMD compared to young healthy normal individuals).
Normal is -1.0 or higher
Osteopenia is -1.0 to -2.5
Osteoporosis is -2.5 or lower
Severe Osteoporosis is -2.5 or lower with fracture
At present for measuring BMD (Bone Mineral Density), the gold standard is DXA (Dual Energy X-Ray Absorptiometry). Others available are Quantitative Computed Tomography (QCT), peripheral devices of X-Rays, ultrasound-based devices, etc.
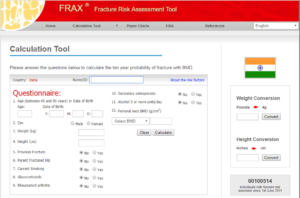
FRAX is a WHO Fracture Risk Assessment Tool. FRAX Scores are calculated by a web-based tool filled by answering questions. They are important and significant for 10 years risk probability of fractures. (Hip fractures – 3% or more, all other fractures – 2% or more; become significant). The advantage of FRAX is fewer younger patients at low 10 Year Risk will be treated and more older patients at higher 10 Year Risk will be treated.
Blood tests for Osteoporosis treatment and finding early secondary factors are – S.Calcium, S.Phosphorus, S.Alkaline Phosphatase, Vit. D3, PTH, S.Creatinine & Urine Routine. Best bone markers in blood are P1NP (Procollagen Type 1 – N – Terminal Propeptide) for formation and CTX1 (Beta Cross – Telopeptide) for resorption.
For males below 50 years, pre-menopausal women and children DO NOT use T-Score for diagnosis of Osteoporosis. Always use Z-Score and when Z-Score is -2.0 or lesser then it is called “Lower than expected” hence better NOT to advise BMD DXA as a routine test for all age groups or for aches and pains. Only for post-menopausal females and males older than 50 years should T-Score be considered in diagnosing Osteoporosis. In children and adolescents, diagnosis of Osteoporosis is NOT on densitometric criteria alone. It is clinically significant history of fractures (long bone fractures of lower extremities &/or vertebral compression fractures &/or two or more long bone fractures of upper-extremities) with a BMD Z-Score of -2.0 or lower.
Low densitometry is not the ONLY cause of Osteoporotic fractures. Other associated problems of neurologic status, balance/gait abnormalities, poor proprioception play a negative influence and increase the risk of fracture. However, the most commonly missed associated problem is SARCOPENIA. Sarcopenia is less muscles (girth & strength). It can be seen in DXA studies as less than 20% of lean mass; & also, as the grip strength of less than 20Kg in females and less than 30Kg in males; &/or speed of walk in 10mins is less than 0.8m/s.
Treatment of Osteoporosis:
- Irrespective of the drugs chosen (Anti-Resorptive &/or Anabolic Pro-Osteoblastic drugs), the common components of treatment are –
- Calcium & Vit.D replete system (Supplementation &/or dietary)
- Walking, Sun bath & Weight bearing exercises
- Improving muscle strength, proprioception & balance
- Prevention of Falls: Remove clutter from the floor, apply grab handles in bathroom/toilets/stairs, keep non-slip floor mats, improve ergonomics of furniture, etc.
- 2. Bisphosphonates (Anti-Resorptive drugs – Anti Osteoclastic) –
The recommendation is NOT to start in pre-menopausal women, males younger than 50 & children.
They have to be started when BMD DXA T-Scores are lesser than -2.0 with fragility fractures or clinical states of higher risk of fractures or T-Scores of -2.5 and below without previous fracture.
Alendronate (70mg) oral – one per week OR Zoledronate (5mg) intravenous infusion – one per year are similar in effectiveness and are preferred over Ibandronate (150mg) – one per month or Resindronate (35mg) – One per week.
Bisphosphonates are contra-indicated if there is preexisting renal impairment (raised creatinine), hyperparathyroidism (primary or secondary).
CORRECT calcium and Vit.D depleted states BEFORE starting Bisphosphonates.
DRUG HOLIDAY from Bisphosphonates is very essential to prevent frozen bone phenomenon & subsequent atypical Bisphosphonates induced fractures. It is to be taken after 4-5 years in mild risk & stable patients and upto 10 years in high risk patients (Eg. GIOP).
REINSTATING Bisphosphonate therapy is to be done only if there is definite declining BMD scores and rising resorption markers (Eg. CTX1) over a period of 2 years of more.
- CALCITONIN Nasal Spray is anti-resorptive. It is now limited in use for “Analgesic” effect in acute Osteoporotic vertebral wedge-compression fractures. Not to be used more than 15 days (present guidelines).
- TERAPERATIDE (injectable Parathormone synthetic analogue). It is a pro-osteoblastic, hence anabolic agent for bone formation. 20µg to 40µg daily subcutaneous injection (patient self administered) for 18 months to max 24 months daily.
It is CONTRAINDICATED in Hyperparathyroidism & Hypovitaminosis D until they are treated and corrected. (So do a BMD DXA, S.Calcium, Vit.D, PTH before starting Teraperatide).
It is recommended to start Teraperatide in T-Scores lesser than -3.5 and/or multiple fragility fractures.
Combination therapy: Teraperatide followed by Bisphosphonate is preferred.
- DENOSUMAB (is a RANK-Ligand fully human monoclonal antibody): It is antiresorptive in nature and used as 60mg subcutaneous injection every 6 months. Till now no limit is set in the number of years it can be used (max use reported is upto 10 years). This is a drug to be used after the use of Bisphosphonate & Teraperatide. It is not to be used as a primary drug yet. Its effect wears off very fast after stopping.
- Other drugs are:
Raloxifene (SERM), Strontium Ranelate, HRT (Estrogen), Bazedoxifene, etc.
FOLLOW-UP studies of BMD are not just to compare T-Score but to measure BMD (Eg. Lumbar spine score of 0.756g/cm2 in 2017 is now gone to 0.781g/cm2 in 2019). So, the difference in the real value is important. Change is considered SIGNIFICANT if there is atleast 0.028g/cm2 in lumbar spine, 0.033g/cm2 in total hip & 0.060g/cm2 in neck femur. The LSC (Least Significant Change) is specific to each center and machine & for LS Spine is 1-2% and for hip 2-3%. The follow-up should be done from the same DXA machine and center. It should be atleast 1 year apart for it to be of value to see the real effectiveness of therapy.
Other things to Remember:
- Low calcium intake and Vit.D deficiency should be corrected in all patients
- Z-Score more negative than T-Score – Start thinking of Osteomalacia
- Low BMD but NOT Osteoporosis is seen in Osteomalacia, Osteogenesis Imperfecta, Renal bone disease, Multiple Myeloma & Bone marrow proliferative disorders.
- Bone formation reduces with very high protein intake, very high cola-drink consumption & very high salt intake
Vit.D & Calcium:
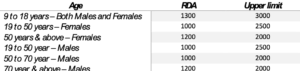
Vit.D daily requirement for maintenance in Vit.D replete system is 1000 IU to upper limit 2000 IU but clinical judgement is necessary (AACE Response to IOM).
Calcium intake in mg (dietary or supplementation) (Institute of Medicine 2011 Dietary reference)

-Dr. Pradumna S. Mamtora
MS Orth., D. Orth.
Consulting Orthopaedic Surgeon
Sunflower Diagnostics | KLS Memorial Hospital | Bhartiya Arogya Nidhi Hospital